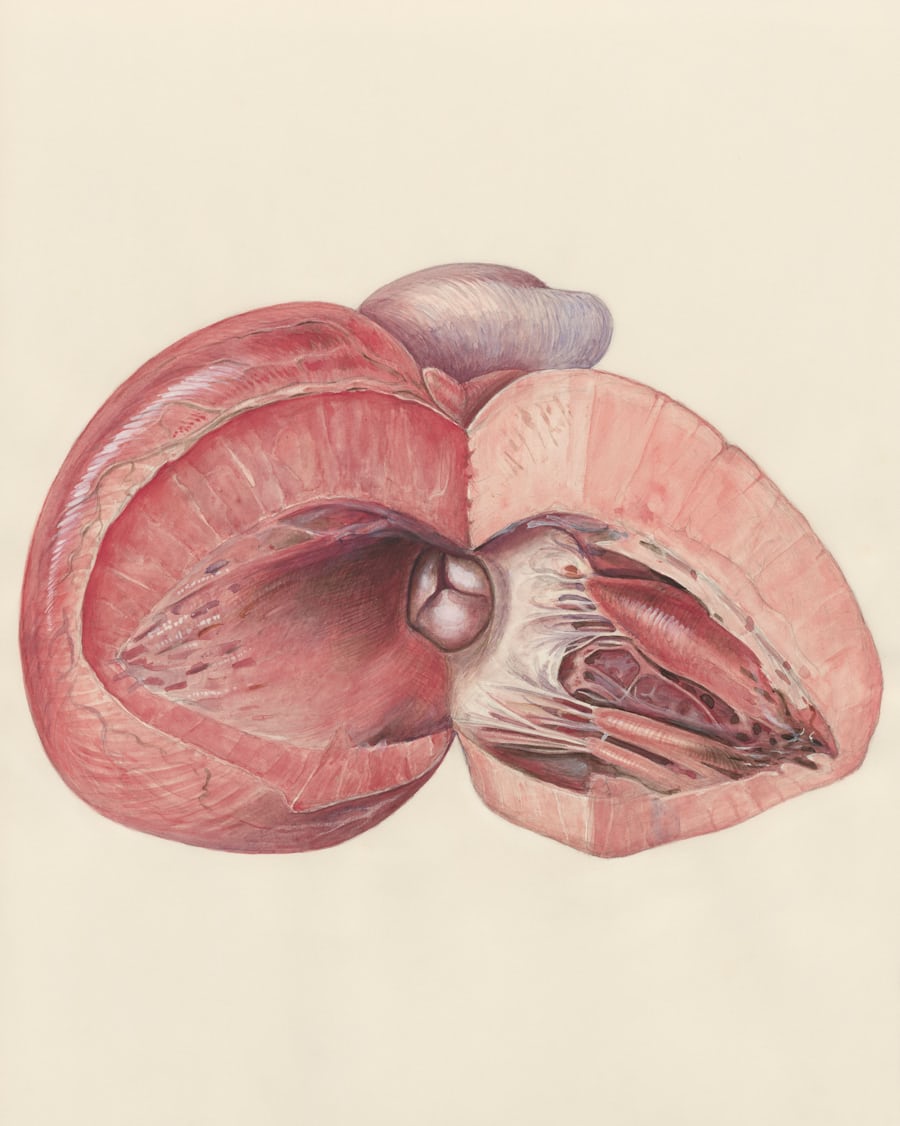
Orchitis: An Overview of Testicular Inflammation
Orchitis is an inflammatory condition affecting one or both testicles, often causing pain and swelling. It can result from either a bacterial or viral infection, with the mumps virus being a historically significant cause. Prompt medical evaluation is crucial to determine the underlying cause and receive appropriate treatment, as some conditions with similar symptoms, like testicular torsion, require immediate surgical intervention.
Causes and Risk Factors:
Orchitis can be broadly categorized based on its cause:
Bacterial Orchitis: This form often develops from an infection spreading from the epididymis, the tube that stores and carries sperm. This is known as epididymo-orchitis. The most common culprits are sexually transmitted infections (STIs) like chlamydia and gonorrhea, particularly in sexually active men. In other cases, bacteria from the urinary tract can lead to orchitis, especially in men with urinary tract abnormalities or those who use a urinary catheter.
Viral Orchitis: The mumps virus is the most well-known viral cause of orchitis. It typically develops in post-pubertal males who contract the mumps. Fortunately, the widespread use of the measles, mumps, and rubella (MMR) vaccine has significantly reduced the incidence of mumps-related orchitis.
Key Symptoms:
The onset of orchitis symptoms can be sudden and may include:
Pain and tenderness in one or both testicles, which can range from mild to severe.
Swelling and a feeling of heaviness in the scrotum.
Redness or warmth of the scrotum.
Fever and chills.
Nausea and vomiting.
General feeling of illness (malaise).
In some cases, pain during urination or ejaculation, and blood in the semen may occur.
Diagnosis and When to Seek Help:
A doctor will typically diagnose orchitis based on a physical examination and a review of the patient’s medical history. The examination will involve checking for testicular swelling, tenderness, and signs of infection.
To confirm the diagnosis and rule out other conditions, the following tests may be ordered:
Urine and Urethral Swab Tests: To check for bacteria and STIs.
Blood Tests: To look for signs of infection.
Ultrasound: This imaging test is crucial to differentiate orchitis from testicular torsion, a medical emergency where the spermatic cord twists, cutting off blood flow to the testicle. An ultrasound can visualize blood flow to the testicles.
It is essential to seek immediate medical attention for any sudden or severe testicular pain.
Treatment Approaches:
Treatment for orchitis depends on the underlying cause:
Bacterial Orchitis: Antibiotics are the primary treatment. The specific antibiotic and the duration of treatment will depend on the bacteria identified or suspected. It is crucial to complete the full course of antibiotics, even if symptoms improve, to ensure the infection is fully eradicated. If an STI is the cause, sexual partners should also be treated.
Viral Orchitis: Since antibiotics are ineffective against viruses, treatment for viral orchitis focuses on relieving symptoms. This includes:
Rest.
Applying cold packs to the scrotum to reduce swelling and pain.
Elevating the scrotum using a supportive garment.
Over-the-counter pain relievers, such as ibuprofen or naproxen.
Potential Complications and Prevention:
While most cases of orchitis resolve with appropriate treatment, potential complications can include:
Testicular Atrophy: The affected testicle may shrink in size.
Scrotal Abscess: A collection of pus can form in the scrotum.
Infertility: In rare cases, especially if both testicles are affected, orchitis can impact fertility.
The most effective way to prevent viral orchitis is through vaccination against mumps. Practicing safe sex, including the use of condoms, can significantly reduce the risk of bacterial orchitis caused by STIs.